Causes and Risk Factors of Cauda Equina Syndrome
Cauda Equina Syndrome (CES) is an exquisite clinical emergency that happens when the nerve roots in the Lower Spinal Region; cauda equina are compressed. These nerves specifically are very important in controlling the bladder, bowel movement, and movement of the lower limbs. When compressed, it causes unemployment effects with consequences such as permanent nerve damage. There is a need to understand what causes CES to easily recognize possible factors that might lead to it, look for early medical attention to avoid outcomes of the condition, and even avoid possible lifelong effects of the condition.
What is Cauda Equina Syndrome?
 Cauda Equina Syndrome arises because of severe compression or inflammation of nerves in the lumbar spine called the cauda equina. These nerves are linked in a way that can be named by their Latin name, cauda equina which means a horse’s tail. They carefully send signals from and to the brain with special emphasis on controlling the movement and sensation below the belt. When compressed, such nerves are unable to perform tasks they were supposed to, resulting in disorders such as excruciating lower back pains, loss of sensations, and even bowel and bladder incontinence. If the condition of the canal is not treated soon then the canal becomes unleachable which is very destructive.
Cauda Equina Syndrome arises because of severe compression or inflammation of nerves in the lumbar spine called the cauda equina. These nerves are linked in a way that can be named by their Latin name, cauda equina which means a horse’s tail. They carefully send signals from and to the brain with special emphasis on controlling the movement and sensation below the belt. When compressed, such nerves are unable to perform tasks they were supposed to, resulting in disorders such as excruciating lower back pains, loss of sensations, and even bowel and bladder incontinence. If the condition of the canal is not treated soon then the canal becomes unleachable which is very destructive.
Common Causes of Cauda Equina Syndrome
Cauda Equina Syndrome may be caused by some conditions that put pressure on the nerves in the region known as the cauda equina.
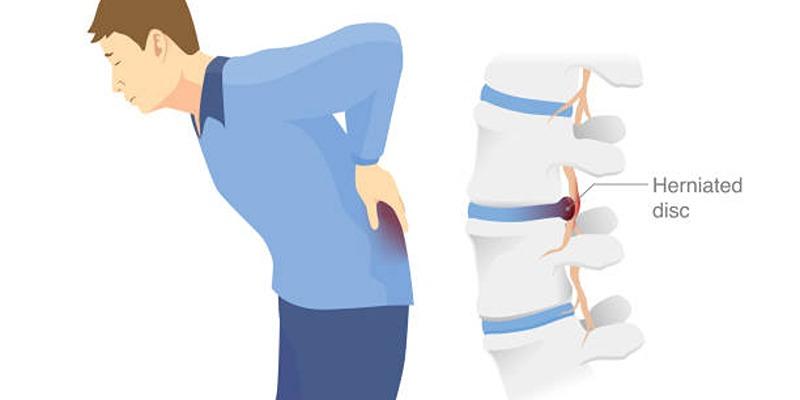
1. Herniated Disc
One of the major contributors to CES is the herniated disc, most especially in the lumbar region. Spinal disc herniation is a condition whereby the soft, jelly-like interior of a disc is squeezed through a tear in its tough exterior and compresses nerves. Although most of the herniated discs are generally mild, a severe displacement of the disc in the lumbar section will also affect the cauda equina nerves which results to CES. This condition tends to happen suddenly and it is a serious condition that always needs the attention of a doctor to avoid severe damage.
2. Spinal Stenosis
Spinal stenosis happens when the space within the spinal canal becomes restricted, leading to pressure on the spinal cord and nearby nerves. This condition is often linked to age-related changes, such as arthritis or the development of bone spurs. If the narrowing occurs in the lower spine, it can impact the cauda equina nerves, increasing the risk of symptoms associated with cauda equina syndrome (CES). Older adults are particularly susceptible to spinal stenosis, making it a common contributing factor to this serious condition.
3. Traumatic Spinal Injury
Severe trauma, such as a car accident, fall, or sports injury, can cause fractures, dislocations, or other damage to the lumbar spine. This type of injury may immediately compress the cauda equina nerves, leading to CES. In some cases, swelling or bleeding within the spinal canal following the injury can exacerbate the pressure on the nerves.
4. Tumors
Spinal tumors, whether benign or malignant, can grow within or near the spinal canal. As they increase in size, they may press on the cauda equina nerves, causing symptoms of CES. Early detection of spinal tumors is crucial for preventing severe complications, as they often require surgical removal or other treatments to relieve the pressure on the nerves.
5. Epidural Hematomas or Abscesses
An epidural hematoma is a collection of blood outside the spinal cord, while an epidural abscess is a buildup of pus caused by an infection. Both conditions can occur in the lumbar region and compress the cauda equina nerves. Epidural hematomas may result from trauma, spinal surgery, or blood-thinning medications, whereas abscesses typically arise from infections in the body that spread to the spine.
Other Contributing Factors to Cauda Equina Syndrome
Cauda equina syndrome can also develop due to a variety of other factors that impact the lumbar spine and its surrounding structures.
1. Infections
Infections such as spinal tuberculosis, osteomyelitis, or discitis can cause inflammation and swelling in the spinal area. When these infections reach the lumbar spine, they may compress the cauda equina nerves and lead to CES. Early treatment of infections is vital to prevent complications.
2. Degenerative Conditions
Chronic degenerative conditions such as ankylosing spondylitis or other forms of spinal arthritis can lead to changes in the spine’s structure. Over time, these changes may narrow the spinal canal or cause instability, increasing the risk of nerve compression and CES.
3. Surgical Complications
While rare, complications from spinal surgeries can sometimes result in CES. This may occur due to scar tissue formation, instability in the spine, or inadvertent damage to the nerves during the procedure. Monitoring post-surgery symptoms is crucial to identify and address any issues early.
4. Prolonged Severe Trauma
Repeated stress or strain on the lower back over time can contribute to the development of CES. This may include heavy lifting, improper posture during physical activities, or high-impact sports. While these factors alone may not directly cause CES, they can exacerbate underlying conditions like herniated discs or spinal stenosis.
Recognizing the Symptoms of Cauda Equina Syndrome
Identifying the symptoms of CES early is critical for prompt medical intervention. Common symptoms include:
- Severe Lower Back Pain: Intense discomfort that may extend to the hips, thighs, or legs.
- Numbness or Tingling: A loss of sensation, often felt in the legs, buttocks, or groin area, commonly referred to as saddle anesthesia.
- Leg Weakness: Challenges with walking, standing, or moving the legs due to reduced strength.
- Bladder and Bowel Dysfunction: Difficulty controlling urination or bowel movements.
Risk Factors for Cauda Equina Syndrome
While CES can occur in anyone, certain risk factors may increase the likelihood of developing this condition. These include:
1. Age
Older adults are at a higher risk of developing CES due to age-related degenerative changes in the spine, such as spinal stenosis or disc herniation.
2. Obesity
Excess weight places additional pressure on the spine, increasing the likelihood of nerve compression and contributing to conditions that lead to CES.
3. Occupation
Jobs involving heavy lifting, repetitive bending, or prolonged periods of sitting can strain the lower back and increase the risk of developing spinal conditions.
Diagnosis and Treatment of Cauda Equina Syndrome
Diagnosing Cauda Equina Syndrome (CES) requires prompt recognition of its symptoms and a careful evaluation to confirm the condition. Early and accurate diagnosis is critical, as timely treatment can prevent permanent nerve damage and improve outcomes.
1. Diagnosis
Doctors use a combination of physical examinations, imaging tests, and patient history to diagnose CES. MRI scans are the most effective tool for identifying the source and severity of nerve compression.
2. Treatment
The primary treatment for CES is surgical decompression, which aims to relieve pressure on the cauda equina nerves. Early surgery is crucial to prevent permanent nerve damage. In some cases, additional treatments such as antibiotics, anti-inflammatory medications, or radiation therapy may be required, depending on the underlying cause.
3. Recovery and Rehabilitation
Following surgery, physical therapy plays a key role in restoring strength, mobility, and nerve function. Patients may need to relearn basic activities such as walking or controlling their bladder, depending on the severity of the condition.
Preventing Cauda Equina Syndrome
 While some risk factors for CES are unavoidable, there are steps individuals can take to reduce their chances of developing this condition:
While some risk factors for CES are unavoidable, there are steps individuals can take to reduce their chances of developing this condition:
1. Maintain a Healthy Spine
Adopt habits that promote spinal health, such as maintaining proper posture, engaging in regular physical activity, and avoiding activities that strain the lower back.
2. Monitor Chronic Conditions
If you have a history of spinal issues or degenerative diseases, regular check-ups with a healthcare provider can help detect problems early and reduce the risk of complications.
3. Use Proper Lifting Techniques
To avoid unnecessary strain on your spine when lifting heavy objects, be sure to bend your knees and keep your back straight.
Conclusion
Cauda Equina Syndrome is a serious condition that requires immediate medical attention. Understanding its causes, such as herniated discs, spinal stenosis, and trauma, can help in early detection and prevention. By recognizing the symptoms and adopting measures to protect your spine, you can reduce the risk of developing this condition. If you suspect CES, seek medical help promptly to ensure the best possible outcome.