Microscopic Polyangiitis: Symptoms, Causes, And Treatments
Microscopic polyangiitis (MPA) is a rare autoimmune disorder that causes inflammation in small blood vessels, medically known as vasculitis. This inflammation can disrupt the normal functioning of multiple organs, primarily affecting the kidneys, lungs, and skin. However, other systems, such as the nervous and gastrointestinal tract, may also become involved. Left untreated, MPA can lead to life-threatening complications, including irreversible organ damage and chronic health issues.
Understanding its complexities is crucial whether you are experiencing symptoms or seeking reliable information about this condition. This article explores the symptoms, causes, and treatment options for microscopic polyangiitis.
Symptoms of Microscopic Polyangiitis:
MPA symptoms vary based on the organs and systems affected, often making diagnosis challenging. Early recognition is vital to prevent long-term complications.
Kidney Symptoms:
- Hematuria: Blood in the urine, which may be visible or microscopic.
- Proteinuria: Excess protein in the urine, a common sign of kidney inflammation.
- Swelling: Fluid retention in the legs, ankles, or feet.
- Decreased Kidney Function: Progression to kidney failure if left untreated.
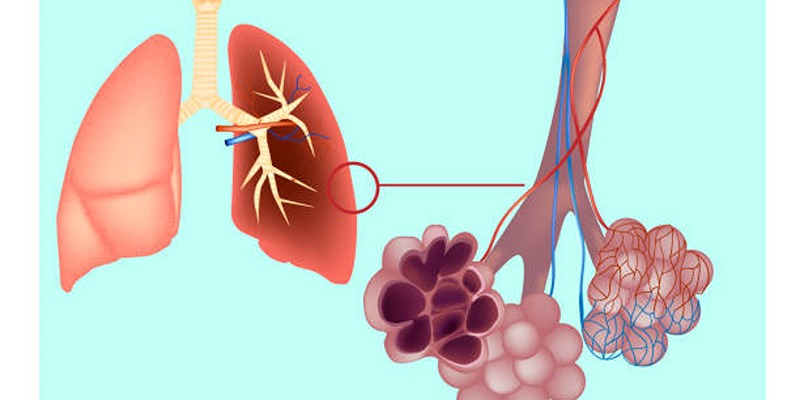
Lung Symptoms:
- Coughing or Hemoptysis: Persistent coughing, sometimes with blood.
- Shortness of Breath: Often a result of alveolar hemorrhage, a severe complication.
- Chest Discomfort: Pain or tightness in the chest.
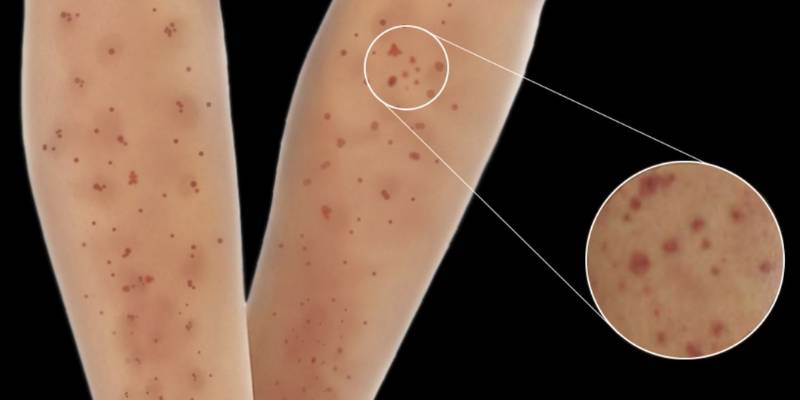
Skin Symptoms:
- Purpura: Red or purple spots caused by bleeding under the skin.
- Painful Nodules: Raised skin lesions that may become ulcers.
- Rashes: Often mistaken for allergic reactions or other skin conditions.
General Symptoms:
- Fever: Low-grade fever during active disease phases.
- Fatigue: Persistent tiredness unrelated to physical activity.
- Unintended Weight Loss: A result of systemic inflammation.
- Joint and Muscle Pain: Often misdiagnosed as arthritis.
- Night Sweats: A symptom of systemic flare-ups.
The diverse presentation of these symptoms often leads to delays in diagnosis, underscoring the importance of consulting a specialist if MPA is suspected.
Causes of Microscopic Polyangiitis:
The precise cause of MPA remains unknown, but it is categorized as an autoimmune disease. Here are some factors that contribute to its development:
Genetic Predisposition:
A family history of autoimmune diseases may increase the likelihood of developing MPA due to genetic factors that make individuals more susceptible to autoimmune reactions.
Environmental Triggers:
Infections, medications, or chemical exposures may act as environmental triggers, activating the disease in genetically predisposed individuals.
Immune System Dysregulation:
Autoantibodies, particularly myeloperoxidase (MPO-ANCA), are often involved in MPA, leading to inflammation of small blood vessels, and contributing to the disease’s progression.
Infections:
Certain bacterial or viral infections, such as respiratory or urinary tract infections, may trigger the immune system to overreact and attack healthy tissues, leading to the development of MPA in susceptible individuals.
Drug Reactions:
Some medications, particularly certain antibiotics, diuretics, and immunosuppressive drugs, have been linked to an increased risk of developing MPA. These drugs can provoke an immune response that results in the inflammation of small blood vessels.
Diagnosis of Microscopic Polyangiitis:
Diagnosing MPA can be challenging because its symptoms often overlap with other forms of vasculitis and autoimmune disorders. A thorough diagnostic approach typically includes the following:
- Blood Tests: Blood tests are essential in diagnosing MPA, as elevated inflammatory markers such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) are commonly found. The presence of myeloperoxidase anti-neutrophil cytoplasmic antibodies (MPO-ANCA) is a key diagnostic indicator for MPA.

- Urinalysis: A urinalysis is performed to detect the presence of blood (hematuria) or protein (proteinuria) in the urine, which are signs of kidney involvement, a common manifestation of MPA.
- Imaging Studies: Imaging techniques such as chest X-rays or CT scans are used to examine the lungs and detect potential complications like alveolar hemorrhage or lung nodules, often seen in MPA patients.
- Biopsy: A biopsy of affected tissues, such as the skin, kidneys, or lungs, may be conducted to confirm the diagnosis. The biopsy typically reveals inflamed small blood vessels, a characteristic of MPA.
- Clinical Evaluation: A thorough clinical evaluation by a healthcare provider is essential in diagnosing MPA. This includes reviewing medical history, assessing symptoms, and ruling out other conditions with similar presentations.
Treatment Options for Microscopic Polyangiitis:
Treatment for MPA aims to suppress the immune system, manage symptoms, and prevent organ damage. It is generally divided into two phases:
Corticosteroids:
High-dose corticosteroids, such as prednisone, are the primary treatment in the induction phase to reduce inflammation rapidly and suppress the immune system’s activity. These medications help control flare-ups and alleviate symptoms.
Immunosuppressive Drugs:
Drugs like cyclophosphamide or rituximab are commonly prescribed to suppress the immune system, inducing remission by reducing the production of harmful autoantibodies that cause inflammation in small blood vessels.
Plasma Exchange (Plasmapheresis):
In severe cases of MPA, plasma exchange may be used to remove harmful autoantibodies from the blood. This procedure helps to reduce inflammation and improve organ function in patients with critical conditions.
Low-Dose Immunosuppressants:
After the induction phase, medications such as azathioprine or methotrexate are prescribed at lower doses to maintain remission, prevent flare-ups, and reduce the need for higher corticosteroid doses, minimizing long-term side effects.
Organ-Specific Treatments:
Depending on the affected organs, patients may need specific treatments, such as oxygen therapy for lung involvement or dialysis for kidney failure, to support organ function and prevent further damage.
Antibiotics:
Antibiotic treatments are used if bacterial infections, such as pneumonia or urinary tract infections, occur in MPA patients. These infections may trigger or exacerbate symptoms of the disease.

Regular Monitoring and Follow-Ups:
Monitoring kidney function, lung health, and inflammatory markers is essential in managing MPA. Regular follow-up visits with healthcare providers help adjust treatment plans, detect relapses, and ensure optimal disease management.
Conclusion
Microscopic polyangiitis is a complex and potentially life-threatening condition that requires prompt diagnosis and a comprehensive treatment plan. From understanding its symptoms to exploring innovative therapies, taking proactive steps can significantly improve outcomes.
Whether you're courting your diagnosis or supporting a loved one, staying informed empowers you to make decisions that promote long-term health. If you suspect MPA or have concerns about your symptoms, consult a healthcare provider today. Early action could make all the difference in managing this rare autoimmune disorder effectively.